“Trauma can include exposures and incidents that anyone would identify as overwhelming, such as physical or sexual assault, combat, major accidents, rape, domestic and community violence, child abuse, and terrorist attacks. It can also include exposures and incidents that are less easily identified, such as rejection, humiliation, neglect, abandonment, bullying and emotional abuse (especially when these occur repeatedly over the course of childhood).”
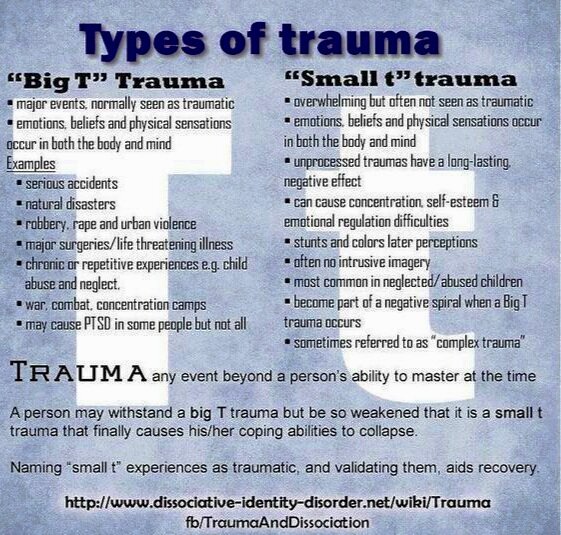
“Big T” and “Small t” traumas are all equally “traumatic”
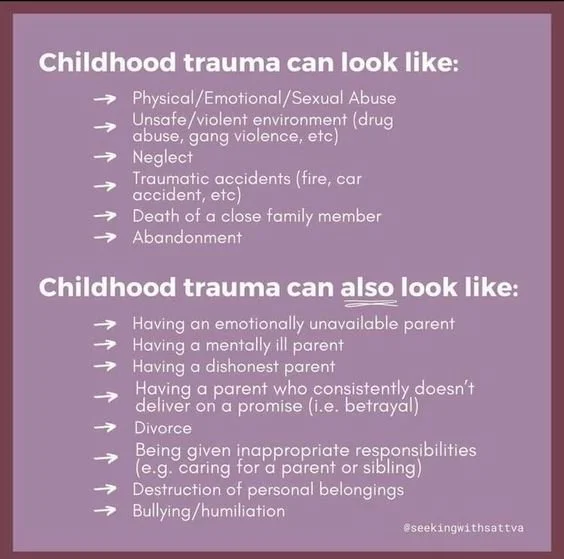
Children experience trauma through commonplace, everyday experiences in their family of origin
In her book, It’s Not You It’s What Happened to You, Dr. Christine Courtois defines trauma as any event or experience (including witnessing) that is physically and/or psychologically overwhelming to the exposed individual. Society seems to have a close minded view on trauma. Most people still think of trauma as “shell shock,” “hysteria” or only resulting from exposure to war or extreme acts of violence (i.e. homicide, suicide, severe physically abusive domestic violence, etc.). These obviously distressing events are referred to as “Big T” Traumas.”
However, consider the “normal,” phase of life events that we all experience as we grow up, such as: divorce, moving or transitions in school (loss); having your first intimate dating relationship end (rejection); parents being mis-attuned to your emotional needs as a child (emotional neglect); being bullied, discriminated against, teased, or judged (humiliation); or growing up with a single or widowed parent (abandonment). Aren’t these commonplace, everyday experiences traumatic, too? Therapists refer to these normal, transitional life events as “small t” traumas.
Because these events are so common, they are often unacknowledged, not recognized or outright dismissed or rejected as traumatic experiences. The fact is distressing life events can either make us grow, adapt and become resilient or—when handled poorly by caregiver/environmental supports—become traumatizing. Consider the experience of Childhood Emotional Neglect (CEN) or being raised by a mentally Ill or substance abusing caregiver. The lingering effects left from such insidious, everpresent events is often more impactful that the Big T traumas of physical or sexual assault.
In Max’s experience, small t traumas, leads to a kind of ‘death by a thousand paper cuts’ and often contribute to mental health disorders, compulsive behaviors and significant dysfunction in managing our sense of safety, control, trust, vulnerability and intimacy in relationships.
How do traumatic experiences impact your physical and mental health?
What is PTSD and what are its symptoms?
Post Traumatic Stress Disorder only became recognized as a psychiatric disorder in 1980. It used to be referred to as ‘hysteria’ or ‘shell shock’ as an explanation for the behavior of military veterans’ psychological reactions to triggering stimuli following war or combat trauma. As discussed above in the section on Big T vs. Small t trauma, society needs to expand it’s understanding of what constitutes a “trauma.”
Childhood Emotional Neglect (CEN) or being raised by a mentally Ill or substance abusing caregiver is often more impactful that physical or sexual assault. All of these experience will evoke the below symptom clusters consistent with PTSD. While all survivors react differently, the three main symptom clusters of PTSD are:
Trauma (of any type) impacts the entire person: body, mind, soul and nervous system
Intrusive experiences (Re-experiencing or Re-living the trauma emotinoally, psychologically, somatically) through the form of flashbacks, nightmares or intrusive thoughts, images or sensory experiences. This cluster is referred to as “intrusive” because the symptoms arise unexpectedly, out of the blue without warning—and “intrude” on your present day experience like an uninvited guest. This can be scary, confusing and make you feel like you’re “going crazy.” In response to these symptoms people express feeling terror, overwhelm, disorientation and powerless. It can feel like a kind of time warp to the traumatic past. It’s hard to think clearly, socialize or plan your day when you are unable to predict what might set these symptoms off.
Avoidance behaviors—including compulsions, obsessions and addictions—used to avoid any reminder, scenario or trigger associated to the original traumatic event(s). This can be conscious as in a driving, or airplane phobia but is often subconscious as in showing up late, procrastinating or abruptly moving in and out of relationships. Avoidance is the core, root problem in most anxiety disorders; which are all about finding ways to avoiding the potential for danger. To learn more take a social anxiety assessment by clicking here
Hyper vigilance, Hyper-arousal or an exaggerated startle response. This looks like jumpiness, feeling "on high alert" all of the time or being ‘stuck in survival mode.’ This can present as paranoia, difficulty concentrating/focusing, inability to relax, chronic body tension/tightness, memory problems, chronic irritability or impulse control problems like sudden aggressive, rageful outbursts or complete shut down/dissociation. People experiencing these symptoms almost always have difficulty sleeping, or significant sleep problems.
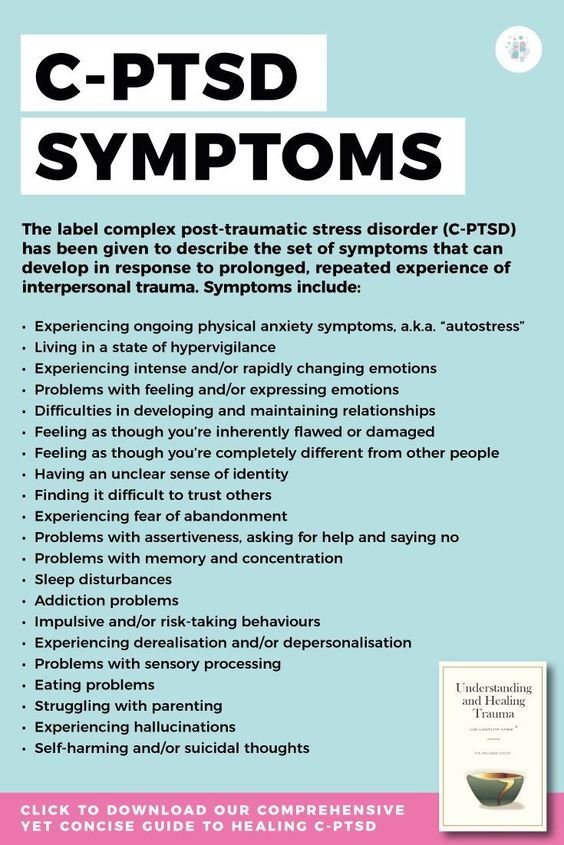
What is Complex ptsd (c-ptsd) or Developmental trauma?
Complex PTSD (also referred to as C-PTSD or Developmental Trauma Disorder) is a more severe form of PTSD, that develops in response to chronic, recurrent, ever-present abuse/neglect and toxic stress experienced during childhood by a trusted attachment figure or caregiver that the child is dependent on to get basic needs met. This form of betrayal or neglect of (caregiving) duty what differentiates C-PTSD from single-incident PTSD.
Children are vulnerable by nature and only grow, develop and mature through life experience. Have you ever heard someone say “you’re just a product of your environment'?” When your childhood home environment and caregivers are chronically unsafe or abusive—like that children of alcoholics, personality disordered parents (i.e. Narcissistic abuse), domestic violence the child feels helpless, hopeless and unable to protect themselves. Because there is no frame of reference or ‘internal working model’ of self the child does not realize nor have the wherewithal to escape. In order to survive and cope with the ever present sense of danger, the human brain then “dissociates” from the present moment, creates an alternative reality and shifts into an “auto-pilot” or “survival mode.” This state is often described as living in a fog; being spacey, detached or ‘being so ADHD,’ etc. In reality, this state of being is a byproduct of the nervous system’s fight/flight/freeze/fawn response to a (perceived) threat to life.
Living in this type of terror and anguish stunts healthy identity formation, relational/social skills and creates an extremely negative view or sense of ‘self.’ Attachment theorist, John Bowlby states: “what can’t be communicated to the mother [during infancy/childhood], cannot be communicate to the self.” This means that if you’re very sense of self cannot devleop when your caregiver is unsafe, erratic or dysfuncitional. There is simply not enough resources to meet both the caregiver and child’s needs. Learn more about C-PTSD here and explore additional symptoms.
“It is the subjective experience of the objective events that constitutes the trauma…The more you believe you are endangered, the more traumatized you will be…Psychologically, the bottom line of trauma is overwhelming emotion and a feeling of utter helplessness. There may or may not be bodily injury, but psychological trauma is coupled with physiological upheaval that plays a leading role in the long-range effects.”